The North Carolina Department of Health and Human Services (NCDHHS) was selected to receive $213 million in federal funds to carry out the first year of the state’s Rural Health Transformation Program (RHTP).
According to a press release from NCDHHS, the award was made in December 2025 by the federal Center for Medicare and Medicaid Services (CMS) after approval of the state’s application. The $213 million was awarded for 2026, and the state will be eligible for annual funding through 2031 contingent on the program’s success in its first year. If awarded, federal funding over the next five years would total $1 billion.
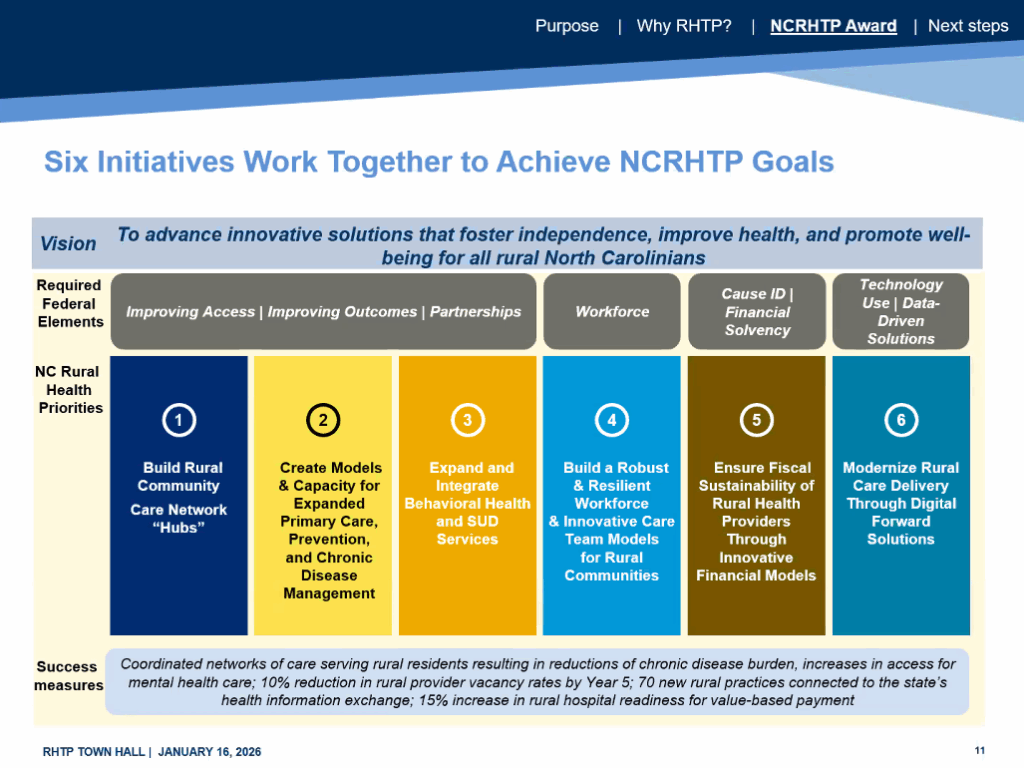
The program will aim to improve health outcomes for the nearly 3 million North Carolina residents living in rural areas by “catalyzing innovative care models, transforming the rural care experience, and creating a sustainable rural delivery system,” per the program’s project abstract.
According to the press release, six interlinked initiatives will guide the RHTP:
- Launch locally governed NC Rural Organizations Orchestrating Transformation for Sustainability (NC ROOTS) Hubs to create centralized comprehensive care for rural residents.
- Expand programs that address prevention, chronic disease management, maternal health, and nutrition.
- Increase access to mental health services, including substance use disorder treatment.
- Invest in the rural health care workforce.
- Help rural providers build the capacity to transition to value-based care models, where providers are paid based on the quality of their care rather than on how many services they provide.
- Enhance technology in health care through artificial intelligence and expanded broadband access.
![]() Sign up for the EdWeekly, a Friday roundup of the most important education news of the week.
Sign up for the EdWeekly, a Friday roundup of the most important education news of the week.
According to the press release, NCDHHS engaged over 400 stakeholders — including rural hospitals, local health departments, Tribal communities, and faith-based organizations — to develop the plan outlined in the application.
State leaders hosted a virtual town hall on Jan. 16 to share the program’s long-term goals and explain how the first year of the program will take shape.
“This funding will improve health care delivery for the more than 3 million North Carolina residents who live in rural communities,” said Gov. Josh Stein at the town hall. “Together, we will set an example here in North Carolina for the nation of what can be accomplished by working together.”
NC ROOTS Hubs will drive rural health care coordination
Debra Farrington, deputy secretary for health at NCDHHS, explained that the first of these six initiatives — NC ROOTS hubs — are key to the first year of the RHTP.
The Hubs, composed of a NC ROOTS Hub Lead and a NC ROOTS Hub Network, will establish locally governed coordinated care networks that make it easier for rural residents to access the care they need. Each Hub Lead will provide centralized governance and support for Hub Network partners, which may include rural hospitals, federally qualified health centers, and private physician practices.
NCDHHS plans to release requests for applications for NC ROOTS Hub Lead organizations by March 2026 and will select six, one for each of the state’s Medicaid Standard Plan regions. Between April and October 2026, NCDHHS says they plan to select and onboard each Hub Lead.
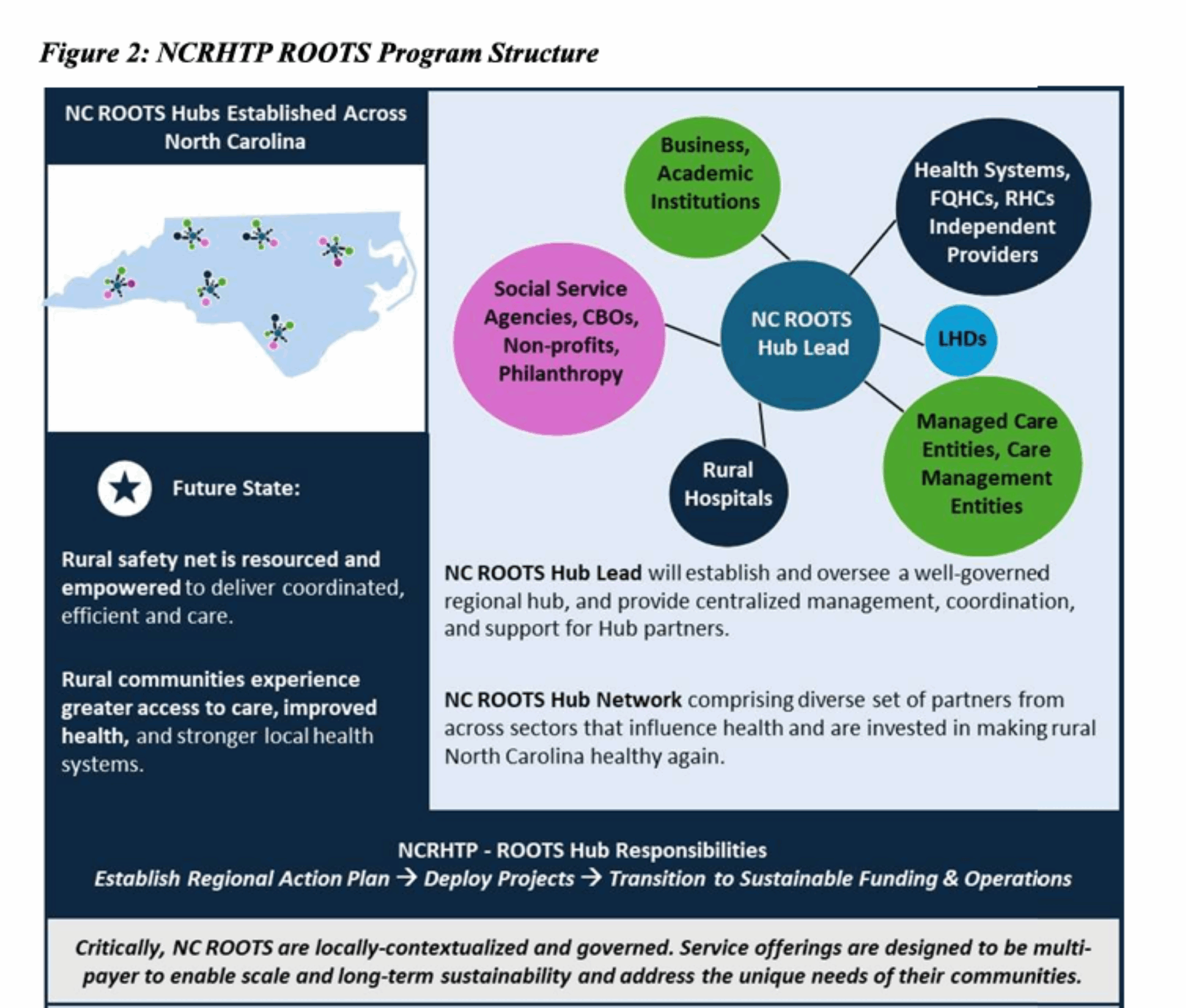
Although Hub Lead applications aren’t open yet, Maggie Sauer, director of the Office of Rural Health at NCDHHS, encouraged interested stakeholders to begin thinking about how their work aligns with the six initiatives outlined in the plan and to begin conversions with any partner organizations about what their collective goals as a Hub Lead would be.
“Make sure people are invited to the table who really can inform a culturally appropriate and regional approach for the needs of your region,” said Sauer.
Investments in the state’s behavioral health infrastructure
Another key RHTP initiative highlighted during the town hall is the state’s plan to strengthen rural behavioral health services through investment in ongoing programs.
The state’s five existing certified community behavioral health clinics (CCBHC) will be central to this work, as they provide a range of substance abuse and mental health services in one physical location. Kelly Crosbie, NCDHHS’s director of the division of mental health, developmental disabilities, and substance use services, described the importance of CCBHCs as “a familiar place in a neighborhood where people can go for access.”
According to the state’s application, the RHTP “will fully expand CCBHC reach to rural communities, coordinated with the regional ROOTS Hubs, and with an enhanced and scaled menu of innovative programs, established infrastructure, and strong commitment to addressing unique rural behavioral health needs.” The document says funding would create between three and four new CCBHCs.
The plan’s behavioral health initiative also plans to increase the number of rural school-based health centers to address critical care gaps. Current programs, such as the NCDHHS partnership with Hazel Health, focus on providing students with telehealth behavioral health services. Crosbie said these digital tools have been an effective way to support students’ mental health.
How NCDHHS defined ‘rural’ for RHTP plans
The town hall included a brief discussion on the program’s definition of a rural county, which the NCDHHS application says is based on Rural Health Grants Eligibility Analyzer and designations implemented by the Health Resources and Services Administration. NC Health News reported that some state legislators have voiced concern about this definition. It resulted in some urban and suburban counties, such as Wake County, being classified as rural, while excluding rural counties such as Burke, Caldwell, and Moore.
Farrington said at the town hall that the definition aligns with federal standards and was chosen to include as many counties as possible — 85 in total — for the purpose of the application.
The RHTP website also states that organizations located in counties not designated as rural in the application are eligible to participate in the program so long as they serve rural populations or support the program’s goals.
“Most importantly, I want to say though that all rural communities will have an opportunity to apply for this funding, and we don’t intend to leave out any rural county,” Farrington added.
NCDHHS leaders shared that the next step for the program is to revise the year one budget and submit it to CMS for final funding approval by Jan. 30. Leaders also said they will continue to engage stakeholders and communicate updates to the public.
The most recent information on the program can be found on the RHTP website, and the public can share input on the program using this feedback form.
Recommended reading