What does a well-functioning health care system require? In the third installment of Rural Talk: A Virtual Advocacy Speaker Series by Rural Counts, leaders and experts in the health care field joined in conversation to talk about rural health amidst a global pandemic.
Alice Schenall, who works with Rural Health Group and moderated the panel, sited the World Health Organization when describing the necessary things needed to create a successful health care system: “a financing mechanism, a well-trained and adequately paid workforce, reliable information for which to base decisions and policies, and well-maintained facilities to deliver the care, and last but not least technologies.”
“The COVID-19 pandemic magnifies the critical issues we face and the need for accessible health care for all North Carolinians. This is especially true for rural communities, low income residents, and communities of color.” – Alice Schenall
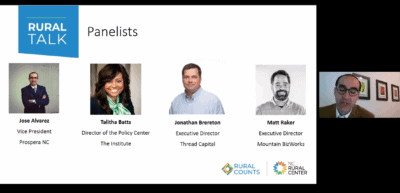
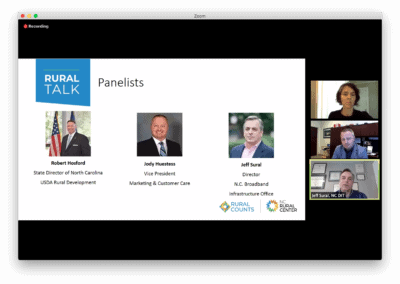
Panelists for this webinar on rural health included Dr. Laura Gerald, president of the Kate B. Reynolds Charitable Trust, Alan Morgan, CEO of the National Rural Health Association, and Allison Owen, deputy director of the Office of Rural Health. At the end, two state legislators joined the call — Sen. Mike Woodard, D-Person, and Rep. Josh Dobson, R-Avery.
The previous two Rural Talk discussions covered broadband access and small businesses. The third discussion can be found below, and if you are interested in joining future conversations, sign up here.
Dire circumstances and silver linings
Of the approximately 2,000 rural hospitals in the United States, 47% of them were operating at a loss back in February before the COVID-19 pandemic hit, according to the Sheps Center at UNC-Chapel Hill. This was before they closed their outpatient and elective procedures, which in many hospitals can account for up to 80% of the revenue, says Morgan.
“So as we’re going into April and the beginning of May, what we’re looking at is the potential to lose more than 400 rural hospitals in the short term.” – Alan Morgan
However, thanks to the CARES Act, this dire projection was avoided. The CARES Act provided necessary funding to keep those doors open and built in time for hospitals to restructure in this new environment.
Morgan wants people to remember, “that while in urban America we’re starting to see this downward trend [in COVID-19 cases], we’re still going to see these surge clusters in rural counties across the US.” This is due to the characteristics found in some rural communities — there tend to be more meat processing plants, interstate connections, and prisons. While the CARES Act has bought rural hospitals some time, they are still in uncharted territory going into the rest of 2020.
All panelists agreed that the social factors that influence our health have exacerbated North Carolinians’ struggles during the COVID-19 pandemic. Things like access to healthy food, broadband, transportation, safe and affordable housing, and interpersonal violence are all growing concerns on their own. On a grander scale, these social determinants are interwoven with overall health and well-being.
Owen mentioned that 80% of today’s health is influenced by factors outside of the clinic. If people aren’t taking care of themselves regularly, which may be harder to do because of COVID-19, those problems may escalate, posing higher bills and more complicated recoveries.
Gerald, who practices medicine in Robeson County, sees a lack of resources and the inequitable distribution of the resources that do exist as major problems.
Robeson has been hit by two hurricanes (Matthew and Florence) in the last four years and struggled with recovery from both natural disasters. Gerald sees disproportionate access to insurance and other health disparities that burden rural communities and result in poor health outcomes.
Kate B. Reynolds Charitable Trust tries to mitigate those health disparities in rural communities with their Healthy Places initiative.
“We’re investing directly in nonprofits in rural areas, who are building capacity, especially marginalized communities, in communities of color, in low income communities. And we’re helping folks to build their own agency in addressing health challenges.” — Dr. Laura Gerald
She says there is a lot we can do to help, but focusing on long-term statewide policy changes are imperative. She believes charity is not enough.
“We should not do with charity what is more effectively and efficiently done with state policy,” Gerald said.
She expressed needing to close the insurance coverage gap so that people can consistently access health care.
“If we, in a pandemic, cannot extend access to health care to those who need it, you know, we all are less safe as a result of that,” Gerald said.
What are some silver linings that the pandemic has brought out? Advancements in telehealth, says Owen.
“We have been able to make strides there that we could not have imagined back in January,” she said.
Owen also pointed out the support the Office of Rural Health is getting from the General Assembly and the partnerships they have been able to create with health care providers.
What policies does Gerald see helping North Carolina move forward? She believes there is a real urgency around Medicaid expansion and that it is important to help build capacity and support nonprofits who are providing community based services and who have direct contact with the people who need access to those services.
“This goes beyond this crisis. If you want to affect policy, and improve the situation in your community, you’ve got to be able to tell your story, tell it effectively, and what it means to your local population.” – Alan Morgan
Recommended reading